A specialized support surface designed to provide comfort and pressure redistribution for patients in healthcare settings. These surfaces utilize air-filled chambers that can be adjusted to customize firmness and alleviate pressure points, enhancing patient well-being during extended periods of bed rest.
Their use is significant in preventing and treating pressure ulcers, a common concern for individuals with limited mobility. By cyclically inflating and deflating air cells, these systems help improve circulation and reduce sustained pressure on vulnerable areas. Historically, the evolution of these support systems has improved patient outcomes and decreased the incidence of hospital-acquired conditions.
The following sections will delve into the types of these surfaces, their operational mechanisms, appropriate usage, maintenance protocols, and factors to consider when selecting the optimal solution for specific patient needs.
Selecting and Utilizing Specialized Support Surfaces
The following guidelines provide essential considerations for choosing and effectively using pressure redistribution surfaces designed for hospital beds.
Tip 1: Assess Patient Risk: Prior to selecting a surface, a thorough risk assessment for pressure ulcer development should be conducted. Factors such as mobility, nutritional status, and existing skin conditions should be evaluated.
Tip 2: Choose Appropriate Type: Determine the most suitable type of surface based on the patient’s risk level and specific needs. Options range from basic alternating pressure models to more advanced low air loss systems.
Tip 3: Verify Correct Inflation: Ensure the support surface is inflated to the manufacturer’s recommended pressure. Improper inflation can reduce effectiveness and potentially harm the patient.
Tip 4: Implement Regular Skin Checks: Conduct frequent skin inspections to identify any signs of pressure damage. Pay close attention to bony prominences such as heels, sacrum, and elbows.
Tip 5: Adhere to Cleaning Protocols: Follow established cleaning and disinfection procedures to maintain a sanitary environment and prevent the spread of infection. Use approved cleaning agents and methods.
Tip 6: Provide Patient Education: Inform the patient and their caregivers about the purpose of the surface and proper usage. This promotes collaboration and ensures adherence to the care plan.
Tip 7: Monitor for Mechanical Issues: Regularly inspect the system for any signs of damage or malfunction. Address any issues promptly to prevent interruptions in pressure redistribution.
Tip 8: Use Appropriate Bedding: Avoid using thick or restrictive bedding that could compromise the effectiveness of the pressure redistribution properties. Opt for breathable, moisture-wicking materials.
Effective implementation of these guidelines can significantly contribute to pressure ulcer prevention and improve patient outcomes in healthcare settings.
The subsequent sections will discuss advanced features and future trends in specialized support surface technology.
1. Pressure Redistribution
Pressure redistribution is a primary function of specialized support surfaces for hospital beds. It aims to mitigate the sustained pressure on bony prominences, thus decreasing the risk of pressure ulcer formation. These surfaces achieve this through interconnected air cells that distribute a patient’s weight across a broader area, preventing localized pressure concentrations. For example, an individual lying supine exerts significant pressure on the sacrum and heels; an appropriately inflated and adjusted support surface can shift this pressure to less vulnerable areas, such as the thighs and upper back. This constant, controlled shifting of pressure prevents tissue ischemia, a leading cause of pressure ulcers.
The effectiveness of pressure redistribution hinges on several factors, including proper inflation, patient positioning, and the specific design of the support surface. Systems with alternating pressure capabilities, for instance, cycle inflation and deflation in different zones to provide periodic relief. Low air loss systems combine pressure redistribution with moisture management, further reducing the risk of skin breakdown. Understanding these mechanisms is vital for healthcare providers, as improper surface selection or usage can negate the intended benefits and compromise patient outcomes. A scenario where a surface is underinflated, for example, would negate the pressure redistribution feature, causing pressure concentrated in bony areas.
In summary, pressure redistribution is an essential feature of advanced support surfaces for hospital beds. Its correct application is a critical component of pressure ulcer prevention protocols. By carefully assessing patient risk factors and selecting appropriate support systems, healthcare professionals can significantly improve patient comfort and reduce the incidence of hospital-acquired pressure ulcers. Continued innovation in support surface technology promises to further enhance pressure redistribution capabilities and improve patient outcomes.
2. Adjustable Firmness
Adjustable firmness is a critical feature in specialized air mattresses used in hospital beds. This adjustability allows healthcare providers to customize the support surface to meet individual patient needs. The ability to modify firmness is essential because patients exhibit diverse body weights, skin integrity levels, and comfort preferences. Without adjustable firmness, a standardized support surface could prove ineffective or even detrimental. A patient with significant weight, for instance, may require a firmer surface to prevent bottoming out, where the body compresses the mattress to the point of contact with the underlying bed frame. Conversely, a patient with fragile skin may benefit from a softer surface to minimize pressure and friction.
The process of adjusting firmness often involves manipulating the air pressure within the internal chambers of the support surface. Lowering the pressure decreases firmness, while increasing it enhances support. Real-world applications of this adjustability include tailoring the surface to accommodate specific medical conditions or post-surgical requirements. A patient recovering from a hip replacement, for example, may require a precisely calibrated level of support to promote proper alignment and reduce pain. Similarly, individuals with existing pressure ulcers may need a softer, more conforming surface to facilitate healing and minimize further tissue damage. This highlights the importance of adjustable firmness and its impact on patient care.
In conclusion, adjustable firmness serves as a cornerstone of effective pressure redistribution and patient comfort in advanced air mattresses. The capabil
ity to fine-tune the support surface not only improves patient outcomes but also enhances the overall efficiency of care. Ongoing research and technological advancements continue to refine these adjustable systems, offering healthcare providers increasingly precise tools for optimizing support and preventing pressure-related complications. The challenges exist in ensuring the precision of these adjustments and the consistency of their application across varied patient populations.
3. Air Cell Technology
Air cell technology is integral to the functionality of specialized support surfaces designed for hospital beds. This technology directly addresses the need for pressure redistribution and patient comfort, serving as a key component in preventing and treating pressure ulcers.
- Pressure Redistribution Through Individual Cells
Air cell technology involves the use of multiple, interconnected air-filled chambers within the mattress. Each cell independently conforms to the patient’s body contours, distributing weight and minimizing pressure concentration on bony prominences. An example includes alternating pressure mattresses, where cells inflate and deflate cyclically to relieve pressure at specific points. The implication is a reduced risk of tissue ischemia, a primary cause of pressure ulcers.
- Adjustable Firmness and Customization
Air cell systems allow for adjustable firmness, enabling healthcare providers to tailor the support surface to individual patient needs. By controlling the air pressure within the cells, the surface can be optimized for different body weights, skin conditions, and comfort preferences. A practical scenario is adjusting the mattress for a patient with delicate skin, reducing pressure to promote healing. The significance lies in enhancing personalized care and improving patient comfort.
- Low Air Loss Functionality for Moisture Management
Some air cell systems incorporate low air loss functionality, which involves the gentle flow of air through the mattress surface. This helps to dissipate moisture and regulate skin temperature, creating a more favorable microclimate for healing. For example, patients with excessive perspiration benefit from this feature, as it helps prevent skin maceration. The consequence is a lower risk of skin breakdown and infection.
- Durability and Infection Control
Air cell mattresses are typically constructed from durable, cleanable materials, facilitating infection control in healthcare settings. The individual cells are often sealed to prevent fluid penetration and contamination. An instance is the use of antimicrobial-treated fabrics, which further reduce the risk of microbial growth. The benefit is an improved level of hygiene and a decreased risk of hospital-acquired infections.
In summary, air cell technology is a vital feature in advanced support surfaces for hospital beds. It facilitates pressure redistribution, adjustable firmness, moisture management, and infection control, all of which are critical for optimizing patient care and preventing pressure-related complications. Continuous advancements in air cell design and functionality hold the potential to further enhance patient outcomes.
4. Patient Comfort
Patient comfort is a crucial consideration in the design and utilization of specialized support surfaces for hospital beds. These surfaces directly impact a patient’s physical and psychological well-being during extended periods of immobility. Inadequate comfort can exacerbate pain, increase anxiety, and disrupt sleep patterns, potentially hindering the healing process. The primary goal of using an air mattress is to reduce pressure points and provide a more supportive and conforming surface compared to standard hospital mattresses. A patient who experiences reduced pain and improved sleep is more likely to adhere to treatment plans and exhibit improved clinical outcomes.
The link between these support surfaces and patient comfort is multifaceted. First, adjustable firmness allows for customization to individual patient needs and preferences. Second, the redistribution of pressure minimizes discomfort associated with prolonged pressure on bony prominences. For example, a patient recovering from surgery may find it challenging to maintain a comfortable position. An adjustable air mattress can be configured to provide optimal support and alleviate pressure in sensitive areas, promoting restful sleep. A patient’s subjective experience of comfort directly influences their overall satisfaction with care, reinforcing a positive therapeutic relationship with healthcare providers. Proper implementation of this intervention requires trained staff capable of assessing the right adjustment and its effects.
In conclusion, patient comfort is not merely a secondary benefit, but an essential component of effective care when using specialized support surfaces. By prioritizing comfort through appropriate selection, adjustment, and monitoring, healthcare professionals can improve patient compliance, enhance overall well-being, and promote favorable clinical outcomes. The challenge lies in continuous evaluation and refinement of these technologies to ensure optimal comfort and functionality for diverse patient populations. Future research should focus on the long-term effects of these support surfaces on patient satisfaction and quality of life.
5. Prevention of Ulcers
The use of specialized support surfaces in healthcare settings is directly linked to the prevention of pressure ulcers, also known as bedsores. These devices are designed to mitigate risk factors associated with prolonged immobility and sustained pressure on vulnerable areas of the body. Effective utilization of these surfaces can significantly reduce the incidence of hospital-acquired pressure ulcers, improving patient outcomes and reducing healthcare costs.
- Pressure Redistribution and Offloading
Air-filled mattresses redistribute a patient’s weight over a larger surface area, decreasing localized pressure on bony prominences such as the sacrum, heels, and hips. This offloading reduces the risk of tissue ischemia and subsequent ulcer formation. Alternating pressure mattresses cycle inflation and deflation, further minimizing sustained pressure in any one area. For example, patients with limited mobility who are confined to bed for extended periods benefit significantly from the constant pressure relief provided by these systems.
- Microclimate Management
Some specialized air mattresses incorporate low air loss technology, which circulates air beneath the patient. This airflow reduces moisture buildup and helps regulate skin temperature, creating a more favorable microclimate and decreasing the risk of skin maceration. Maintaining a dry and cool skin surface is crucial in preventing skin breakdown, particularly for patients who are incontinent or perspire heavily. This assists in reducing the chances of infections.
- Individualized Support and Comfort
Adjustable firmness settings allow healthcare providers to tailor the support surface to individual pat
ient needs, accommodating variations in body weight, skin integrity, and comfort preferences. The capacity to fine-tune the support level ensures optimal pressure redistribution and reduces the risk of bottoming out, where the patient’s body makes contact with the underlying mattress base. For instance, an undernourished patient with fragile skin requires a softer support surface than an obese patient who needs more substantial support. - Early Intervention and Risk Mitigation
The implementation of these support surfaces as part of a comprehensive pressure ulcer prevention protocol, including regular skin assessments and repositioning schedules, can significantly reduce the incidence of pressure ulcers in at-risk populations. Early intervention is critical, as established ulcers are more challenging and costly to treat. By proactively addressing risk factors, healthcare providers can improve patient outcomes and reduce the burden on healthcare systems.
In summary, the utilization of air-filled mattresses is a key component of pressure ulcer prevention strategies. By providing pressure redistribution, microclimate management, individualized support, and enabling early intervention, these surfaces contribute to a reduction in the incidence and severity of pressure ulcers. These factors improve patient care, and improve patient outcomes in hospital settings.
Frequently Asked Questions
The following section addresses common inquiries regarding air-filled mattresses in hospital settings, providing detailed information to facilitate informed decision-making.
Question 1: How does an air-filled mattress differ from a standard hospital mattress?
Air-filled mattresses utilize interconnected air cells to redistribute pressure and conform to a patient’s body, whereas standard mattresses typically consist of foam or innerspring construction. Air-filled models provide enhanced pressure relief and can be adjusted to meet individual patient needs, factors generally lacking in standard mattresses.
Question 2: What factors should be considered when selecting an air-filled mattress for a patient?
Key considerations include the patient’s risk level for pressure ulcer development, mobility status, weight, skin integrity, and any existing medical conditions. Selecting an appropriate surface requires a comprehensive assessment to ensure optimal pressure redistribution and support.
Question 3: How often should an air-filled mattress be cleaned, and what cleaning agents are recommended?
Air-filled mattresses should be cleaned and disinfected between patient uses and routinely as part of a regular maintenance schedule. Manufacturers typically recommend specific cleaning agents compatible with the mattress materials. Harsh chemicals or abrasive cleaners should be avoided to prevent damage.
Question 4: What are the common issues related to the air-filled mattress?
Potential issues can include pump malfunction, air leaks, and improper inflation. A systematic approach is needed to address these. Regular inspection and preventative maintenance are essential. Addressing these issues quickly is crucial to the sustained functionality.
Question 5: What are the potential risks associated with improper use of a support surface?
Improper use, such as incorrect inflation or failure to follow cleaning protocols, can compromise pressure redistribution and increase the risk of pressure ulcers and infection. It is vital to ensure healthcare providers receive appropriate training and adhere to manufacturer guidelines.
Question 6: What is the life expectancy of specialized support surfaces?
The life expectancy of an air-filled mattress depends on factors such as usage frequency, maintenance practices, and the quality of materials. Routine maintenance and timely repairs can help extend the lifespan of the surface. Following manufacturer guidelines ensures longevity of the mattress.
In summary, appropriate selection, maintenance, and utilization of air-filled mattresses are essential for effective pressure ulcer prevention and optimal patient care.
The subsequent section will explore emerging trends and future directions in specialized support surface technology.
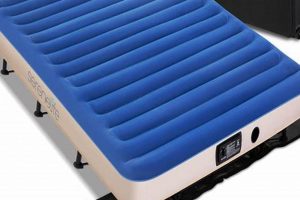
Inflatable Mattress for Hospital Bed
This exploration has detailed the significance of the inflatable mattress for hospital bed as a primary tool in pressure ulcer prevention and enhanced patient comfort. Effective pressure redistribution, adjustable firmness, and advanced air cell technology collectively contribute to improved patient outcomes and reduced healthcare costs associated with hospital-acquired pressure ulcers. The correct selection, use, and maintenance of these systems are paramount.
Moving forward, continued research and development in support surface technology are essential to address the evolving needs of diverse patient populations. Healthcare professionals should remain vigilant in assessing patient risk factors and implementing comprehensive pressure ulcer prevention protocols. The future of patient care depends on continued innovation and a commitment to providing optimal support and comfort for those requiring prolonged bed rest.





![Best Truck Bed Inflatable Mattress [Deals] for Comfortable Sleep Organic & Natural Mattress Buyer’s Guide: Non-Toxic Sleep Solutions Best Truck Bed Inflatable Mattress [Deals] for Comfortable Sleep | Organic & Natural Mattress Buyer’s Guide: Non-Toxic Sleep Solutions](https://mattressworldpa.com/wp-content/uploads/2025/07/th-7233-300x200.jpg)
