A specialized piece of medical equipment designed for patient care, consisting of an adjustable frame and a supportive surface. This apparatus provides a safe and comfortable environment for individuals requiring extended periods of bed rest or medical treatment. It often includes features such as adjustable height, head and foot elevation, and side rails to enhance patient safety and caregiver convenience. The supporting surface, typically constructed from foam, innerspring, or air-filled materials, contributes to pressure redistribution and comfort.
This essential healthcare item plays a vital role in promoting patient recovery and overall well-being. The adjustable features facilitate easier access for medical staff during examinations and treatments, while also allowing patients to find more comfortable positions, reducing the risk of pressure ulcers and improving circulation. Historically, such equipment has evolved from simple cots to sophisticated systems incorporating advanced technology to meet the complex needs of modern healthcare.
The following sections will delve into the various types, features, selection criteria, maintenance, and technological advancements associated with this crucial element of patient care infrastructure. Examining these aspects will provide a comprehensive understanding of its function and significance within the healthcare setting.
Essential Considerations for Optimal Use
This section outlines crucial tips for the effective selection, utilization, and maintenance of the specified equipment to ensure patient safety and longevity of the device.
Tip 1: Proper Weight Capacity Assessment: Always verify that the individual utilizing the apparatus does not exceed the maximum weight capacity specified by the manufacturer. Exceeding this limit can compromise the structural integrity and safety features of the mechanism.
Tip 2: Regular Inspection for Wear and Tear: Conduct routine inspections of the frame, mattress, and all adjustable components. Look for signs of damage, such as cracks, tears, or loose connections. Address any issues immediately to prevent potential hazards.
Tip 3: Optimal Mattress Selection for Pressure Relief: Choose a mattress type appropriate for the individual’s needs and risk factors for pressure ulcers. Consider factors like material composition, thickness, and pressure redistribution capabilities.
Tip 4: Consistent Cleaning and Hygiene Maintenance: Adhere to a strict cleaning protocol, using approved disinfectants, to minimize the risk of infection. Regularly clean the mattress surface and all exposed parts of the frame. Follow manufacturer’s recommendations for cleaning agents and frequency.
Tip 5: Correct Adjustment Techniques for Patient Comfort and Safety: Familiarize personnel with the proper techniques for adjusting the bed’s height, head and foot elevations, and side rails. Ensure that adjustments are made smoothly and safely to prevent injury to the individual or caregivers.
Tip 6: Secure Side Rail Placement and Operation: Verify that side rails are properly secured and functioning correctly before leaving an individual unattended. Ensure that the individual or caregiver understands how to operate the side rails, if appropriate.
Tip 7: Proper Storage When Not in Use: When not in use, store the frame in a clean, dry environment, protected from extreme temperatures and humidity. This will help prevent damage and extend the lifespan of the equipment.
Adhering to these guidelines will help to maximize the benefits of the equipment while minimizing the risks associated with its use. Consistent attention to these details contributes to a safer and more comfortable environment.
The subsequent discussion will address advanced features and future trends in the design and technology of this essential device.
1. Support
The concept of “Support” in the context of a hospital bed with mattress is paramount. It refers to the ability of the structure and surface to bear weight and provide a stable foundation for the patient, directly influencing patient safety, comfort, and the prevention of secondary complications.
- Structural Integrity
Structural integrity denotes the frames load-bearing capacity and stability. A robust frame, constructed from durable materials like steel, must withstand significant weight and repeated adjustments without deformation or failure. Inadequate structural integrity compromises safety, potentially leading to falls or injuries. For instance, a frame with a weakened welding point might collapse under a heavier patient, resulting in serious harm.
- Mattress Load Distribution
The mattresss ability to distribute weight evenly is crucial for pressure relief and the prevention of pressure ulcers. A supportive surface conforms to the patients body, minimizing concentrated pressure points. Ineffective load distribution, such as with a sagging or worn mattress, concentrates pressure on bony prominences, increasing the risk of skin breakdown. Specialty mattresses with air or foam cells are designed to enhance load distribution and reduce pressure.
- Side Rail Stability
Side rails contribute significantly to patient support by providing a stable handhold for repositioning and preventing falls. Rails must be securely attached to the frame and capable of withstanding lateral force without detaching or collapsing. Loose or poorly designed side rails present a serious fall risk, particularly for patients with impaired mobility or cognitive function.
- Adjustability Mechanisms
The mechanisms that enable height and positional adjustments must provide reliable and consistent support throughout their range of motion. These mechanisms, often involving electric motors or manual cranks, must maintain the selected position securely without slippage or instability. Malfunctioning adjustment mechanisms can create unstable surfaces, increasing the risk of patient falls and caregiver strain.
The interplay of structural integrity, mattress load distribution, side rail stability, and reliable adjustment mechanisms collectively defines the “Support” provided by a hospital bed with mattress. Each facet directly contributes to patient safety, comfort, and the prevention of secondary complications, underscoring the importance of carefully evaluating these elements during procurement and maintenance.
2. Adjustability
Adjustability is an integral attribute of a hospital bed with mattress, directly influencing patient comfort, caregiver ergonomics, and the efficacy of medical treatments. The capacity to modify the bed’s configuration enables healthcare professionals to optimize patient positioning for various therapeutic interventions, examinations, and personal care activities. Without adjustability, provid
ing adequate care and promoting patient recovery becomes significantly more challenging. For example, elevating the head of the bed can aid respiratory function in patients with pulmonary conditions, while raising the foot of the bed can improve circulation in individuals with edema.
Different types of adjustability mechanisms cater to diverse patient needs and clinical settings. Electric beds allow for effortless and precise adjustments via remote control, benefiting both patients and caregivers. Manual beds, while less convenient, offer a more cost-effective solution in certain environments. The adjustable features typically include height, head elevation (Fowler’s position), and knee elevation. These adjustments facilitate easier transfers, reduce the risk of falls, and promote independence for patients with limited mobility. The selection of a bed with appropriate adjustability features should be based on a comprehensive assessment of the patient’s medical condition, physical capabilities, and the specific requirements of their care plan.
In summary, the adjustability of a hospital bed with mattress is a critical factor in delivering optimal patient care. It allows for customized positioning to address specific medical needs, enhance comfort, and improve caregiver efficiency. While challenges may arise in balancing cost considerations with the need for advanced features, prioritizing adjustability remains essential to maximizing the therapeutic benefits of this equipment. The ongoing development of more intuitive and versatile adjustment mechanisms promises to further enhance the role of hospital beds in promoting patient well-being and recovery.
3. Hygiene
Hygiene, in the context of a hospital bed with mattress, represents a critical aspect of infection control and patient safety. The bed and mattress serve as potential reservoirs for microorganisms, underscoring the necessity of rigorous cleaning and disinfection protocols. Maintaining hygiene minimizes the risk of healthcare-associated infections (HAIs) and promotes a safe and sanitary environment for patient recovery.
- Material Selection and Antimicrobial Properties
The choice of materials used in the construction of the mattress and bed frame significantly impacts hygiene. Non-porous surfaces, such as vinyl or treated fabrics, are easier to clean and disinfect compared to porous materials. Some mattresses incorporate antimicrobial agents to inhibit the growth of bacteria and fungi. For example, mattresses with silver-ion infused covers can reduce microbial colonization. This feature can have implications in long term care settings, such as nursing homes, where patients may be at higher risk for infection and where frequent cleaning may be a challenge.
- Cleaning and Disinfection Protocols
Established cleaning and disinfection protocols are essential for maintaining hygiene. These protocols involve the regular use of hospital-grade disinfectants to eliminate pathogens from the bed frame and mattress surface. Proper cleaning techniques, including thorough wiping and adherence to contact times, are crucial for effective disinfection. Neglecting these protocols can lead to the transmission of infections among patients. For instance, norovirus outbreaks have been linked to inadequate disinfection of surfaces in healthcare facilities.
- Fluid Resistance and Barrier Protection
Mattress covers designed with fluid-resistant or waterproof barriers prevent bodily fluids from penetrating the mattress core. This barrier protection minimizes the risk of contamination and facilitates easier cleaning. Fluid penetration can create a breeding ground for bacteria and compromise the integrity of the mattress. Incontinence pads or specialized mattress covers are often employed to enhance barrier protection and maintain hygiene.
- Inspection and Maintenance
Regular inspection and maintenance of the bed frame and mattress are essential for identifying and addressing potential hygiene issues. Damaged or torn mattress covers should be repaired or replaced promptly to prevent fluid penetration. Loose or damaged bed frame components should be addressed to maintain structural integrity and facilitate thorough cleaning. Neglecting maintenance can compromise hygiene and increase the risk of infection.
The various facets of hygiene, including material selection, cleaning protocols, fluid resistance, and maintenance, collectively contribute to minimizing the risk of infection and promoting a safe patient care environment. A comprehensive approach to hygiene, encompassing all of these elements, is essential for ensuring the effective use of a hospital bed with mattress and protecting patient well-being.
4. Durability
Durability, in the context of a hospital bed with mattress, denotes the capacity of the apparatus to withstand prolonged use and maintain its functional integrity over an extended period. It is a critical factor in healthcare settings, impacting both the cost-effectiveness and the safety of patient care.
- Frame Construction and Material Strength
The frame’s construction and the materials employed directly influence its resistance to wear and tear. High-gauge steel frames, reinforced with welding at critical stress points, exhibit greater durability than those constructed from lighter materials or with less robust joinery. For instance, a bed frame subjected to repeated adjustments and heavy loads will demonstrate its durability through the absence of bending, cracking, or joint failure. This aspect becomes particularly relevant in bariatric units, where beds must support significantly higher weights.
- Mattress Material Resistance to Degradation
The mattress material must resist degradation from repeated use, cleaning, and exposure to bodily fluids. High-density foam, innerspring systems with tempered coils, and specialized air-filled mattresses exhibit varying degrees of durability. A mattress that prematurely loses its shape, develops indentations, or becomes susceptible to tearing compromises patient comfort and pressure redistribution capabilities. The selection of a mattress material should consider the anticipated frequency of use, cleaning protocols, and the specific needs of the patient population.
- Mechanical Component Longevity
Mechanical components, such as motors, actuators, and control systems, must function reliably over an extended lifespan. These components are subject to constant use and must withstand the stresses associated with height adjustments, head and foot elevation, and other positional changes. High-quality components, coupled with regular maintenance, contribute to the overall durability of the hospital bed. Failure of these components can lead to operational disruptions and potential safety hazards.
- Surface Finish Resistance to Corrosion and Damage
The surface finish applied to the frame and components must resist corrosion, scratching, and other forms of damage. Powder-coated finishes, for example, provide a durable protective layer that withstands repeated cleaning and exposure to harsh chemicals. A compromised surface finish can lead to rust, which weakens the frame and creates a breeding ground for bacteria. Regular inspection and maintenance of the surface finish are essential for maintaining the bed’s aesthetic appeal and structural integrity.
These facets of durability are interconnected and collectively determine the overall lifespan and performance of the hospital bed with mattress. Prioritizing durability in the selection and maintenance of this equipment translates to long-term cost savings, improved patient safety, and enhanced operational efficiency within healthcare facilities.
5. Safety
The integration of safety features within the design and operation of hospital beds with mattresses directly mitigates risks associated with patient falls, entrapment, and other potential injuries. A primary concern is fall prevention, addressed through adjustable bed height to facilitate safe ingress and egress, as well as the incorporation of side rails. Incorrectly positioned or malfunctioning side rails, conversely, can present an entrapment hazard. For example, a patient attempting to exit a bed with improperly secured rails might become lodged between the rail and the mattress, leading to injury or, in extreme cases, death. Another critical aspect is the selection of appropriate mattress materials. Mattresses lacking adequate support or pressure redistribution can contribute to the development of pressure ulcers, creating a safety concern that extends beyond the immediate risk of injury.
Furthermore, electrical safety is paramount in electrically adjustable beds. Malfunctioning electrical components can pose a shock hazard to both patients and staff. Regular maintenance and adherence to electrical safety standards are crucial in preventing such incidents. The practical significance of understanding these safety considerations extends to healthcare facility procurement processes, where selecting beds with certified safety features and adhering to rigorous maintenance schedules are essential. Incident reporting systems provide valuable data for identifying potential safety flaws in bed design or operational procedures, allowing for proactive adjustments to minimize patient risk. Training healthcare staff on proper bed operation and safety protocols is similarly vital to promote patient well-being and prevent avoidable injuries.
In summation, the multifaceted relationship between safety and hospital beds with mattresses underscores the importance of proactive risk management in healthcare settings. While technological advancements continue to enhance safety features, the effectiveness of these measures is contingent upon proper implementation, maintenance, and staff training. The challenge lies in balancing the need for advanced functionality with the paramount concern of patient safety, ensuring that these essential pieces of equipment contribute to a secure and healing environment.
6. Positioning
The therapeutic benefit derived from a hospital bed with mattress is inextricably linked to the capacity to facilitate precise and adaptable positioning. This positioning capability directly influences physiological processes, including respiration, circulation, and pressure distribution. For instance, elevating the head of the bed (Fowler’s position) can improve lung expansion and oxygenation in patients with respiratory distress, while Trendelenburg positioning (tilting the bed with the head lower than the feet) can enhance venous return in individuals experiencing hypotension. Without the ability to achieve these specific positions, the potential for optimized patient outcomes is significantly diminished. The cause-and-effect relationship is clear: appropriate positioning, enabled by the design of the hospital bed, leads to improved physiological function and reduced risk of complications.
Effective positioning, made possible through hospital bed adjustability, extends beyond acute medical interventions. It plays a crucial role in preventing pressure ulcers, particularly in immobile or neurologically impaired patients. Regular repositioning, facilitated by the bed’s features, redistributes pressure away from bony prominences, minimizing the risk of tissue breakdown. Lateral rotation therapy, often employed in intensive care units, utilizes specialized beds to automatically rotate patients from side to side, further reducing the incidence of pressure ulcers and promoting pulmonary hygiene. The practical significance of this is evident in reduced hospital stays, decreased healthcare costs associated with treating pressure ulcers, and improved patient quality of life. Furthermore, appropriate positioning can alleviate pain and discomfort, promoting relaxation and sleep, which are essential components of the healing process.
In conclusion, positioning is not merely an ancillary feature of a hospital bed with mattress; it is an integral component that directly impacts patient outcomes and overall well-being. Challenges remain in ensuring that all healthcare settings have access to beds with the necessary positioning capabilities and that staff are adequately trained in their proper utilization. The continued development of innovative positioning technologies and protocols holds the promise of further enhancing the therapeutic benefits of hospital beds, contributing to improved patient care and reduced healthcare burdens.
Frequently Asked Questions
This section addresses common inquiries regarding hospital beds with mattresses, providing concise and factual information to aid understanding and decision-making.
Question 1: What distinguishes a hospital bed with mattress from a standard bed?
A hospital bed, unlike a standard bed, incorporates adjustable features such as height, head, and foot elevation, enabling tailored patient positioning. The inclusion of side rails and specialized mattresses further enhances safety and comfort, accommodating specific medical needs.
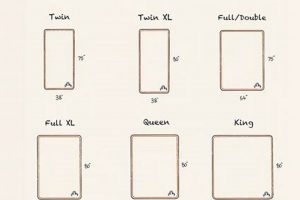
Question 2: What are the primary considerations when selecting a hospital bed mattress?
Key factors include pressure redistribution capabilities, material composition (foam, innerspring, air), fluid resistance, and compatibility with the bed frame. Patient weight, risk of pressure ulcers, and specific medical conditions should also inform the selection process.
Question 3: What is the recommended cleaning protocol for a hospital bed with mattress?
Regular cleaning with hospital-grade disinfectants is essential. Mattresses should be wiped down, ensuring all surfaces are treated according to the disinfectant’s contact time requirements. Bed frames should be similarly cleaned, paying attention to crevices and adjustable components.
Question 4: How frequently should a hospital bed with mattress undergo maintenance checks?
Routine inspections, ideally conducted monthly, should assess the bed frame for structural integrity, functionality of adjustable components, and the mattress for signs of wear or damage. Electrical components should be inspected by qualified personnel.
Question 5: What safety features are crucial in a hospital bed with mattress?
Essential safety features include secure and functional side rails, locking mechanisms for wheels, and compliance with electrical safety standards. The bed’s weight capacity should be clearly marked and strictly adhered to.
Question 6: What are the different types of hospital bed mattresses available?
Common types include foam mattresses (memory foam, polyurethane foam), innerspring mattresses, air mattresses (alternating pressure, low air loss), and specialty mattresses designed for specific
conditions such as pressure ulcers.
Understanding these key aspects is critical for ensuring the optimal selection, utilization, and maintenance of hospital beds with mattresses, ultimately contributing to improved patient care and safety.
The subsequent section will address emerging technologies and future trends in hospital bed design and functionality.
Conclusion
This exploration has detailed the essential attributes of a hospital bed with mattress, encompassing support, adjustability, hygiene, durability, safety, and positioning. Each facet contributes to the overall efficacy of the device in promoting patient well-being and facilitating medical interventions. The integration of these features is paramount in ensuring a safe and therapeutic environment.
Continued advancements in hospital bed technology hold the potential to further enhance patient care. Prioritizing informed selection, diligent maintenance, and adherence to safety protocols remains crucial to maximizing the benefits and minimizing the risks associated with this critical element of healthcare infrastructure. Vigilance and ongoing evaluation are essential to ensure the continued optimization of patient outcomes.