A specialized support surface engineered for use on adjustable hospital beds, this device helps manage patient skin integrity and comfort. It achieves this through a system of air-filled bladders that cyclically inflate and deflate, redistributing pressure across the user’s body. This dynamic pressure redistribution minimizes concentrated pressure on bony prominences, reducing the risk of pressure injuries.
The utilization of these surfaces offers several key advantages in patient care. Historically, preventing pressure ulcers relied heavily on frequent repositioning by nursing staff. The technology reduces the need for constant manual adjustments, freeing up staff resources and enhancing patient well-being. Furthermore, the circulation of air within the mattress can help regulate skin temperature and reduce moisture buildup, factors contributing to skin breakdown. These attributes contribute to improved patient outcomes and a more efficient healthcare environment.
The subsequent sections will delve into the specific mechanisms of action, the various types available, the criteria for appropriate patient selection, proper maintenance procedures, and the clinical evidence supporting its efficacy in pressure injury prevention and management within acute and long-term care settings.
Guidance on Utilizing a Low Air Loss Support Surface
The following points offer essential guidance for maximizing the effectiveness and longevity of this support surface.
Tip 1: Patient Selection is Paramount: Conduct a thorough risk assessment to determine appropriate candidates. Consider factors such as immobility, incontinence, nutritional status, and existing skin conditions. This assessment informs the decision to employ this specialized surface.
Tip 2: Ensure Correct Mattress Inflation: Follow the manufacturer’s instructions meticulously to achieve the optimal inflation level. An improperly inflated mattress may not provide adequate pressure redistribution, negating its therapeutic benefits.
Tip 3: Implement a Consistent Skin Care Regimen: Utilize the support surface in conjunction with a comprehensive skin care protocol. Regular skin assessments, gentle cleansing, and the application of appropriate barrier creams are essential adjuncts to pressure ulcer prevention.
Tip 4: Monitor Air Loss and Functionality: Regularly inspect the surface for leaks or malfunctions. A compromised surface compromises its therapeutic effectiveness. Promptly address any identified issues by repairing or replacing the mattress, as necessary.
Tip 5: Educate Caregivers and Patients: Provide clear and concise instructions to all involved regarding the proper operation and maintenance of the device. This ensures consistent application of best practices and promotes optimal patient outcomes.
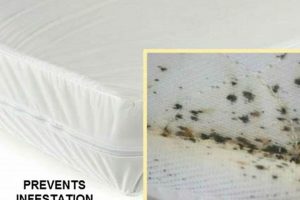
Tip 6: Protect the Mattress Surface: Employ a moisture-wicking, breathable cover to protect the integrity of the mattress. This barrier prevents fluid penetration, simplifies cleaning, and extends the lifespan of the support surface.
Tip 7: Adhere to Cleaning and Disinfection Protocols: Implement rigorous cleaning and disinfection procedures between patient uses, adhering to established infection control guidelines. This is crucial for preventing cross-contamination and safeguarding patient health.
Adherence to these principles maximizes the potential benefits of the surface, contributing to a reduction in pressure injury incidence and improved patient comfort.
The following sections will address further considerations for its integration into comprehensive pressure injury prevention programs.
1. Pressure Redistribution
Pressure redistribution is a fundamental principle in the prevention and management of pressure injuries, and it is the primary mechanism by which a low air loss mattress for a hospital bed exerts its therapeutic effect. By dynamically altering the points of contact and reducing peak pressures on vulnerable areas, this specialized surface mitigates the risk of tissue ischemia and subsequent ulcer formation.
- Alternating Inflation and Deflation Cycles
The core functionality involves cyclical inflation and deflation of individual air bladders within the mattress. This orchestrated process changes the support surface dynamically, preventing prolonged pressure on specific anatomical locations. For example, areas such as the sacrum, coccyx, and heels, which are particularly susceptible to pressure injuries due to their bony prominences and limited subcutaneous tissue, benefit significantly from this continuous shifting of pressure. By minimizing sustained pressure on these high-risk areas, the likelihood of tissue damage is substantially reduced. This cyclical action improves blood flow to tissues that might otherwise be compressed for prolonged durations.
- Immersion and Envelopment
A low air loss system facilitates immersion, allowing the patient to sink slightly into the mattress. This increases the contact area between the patient and the support surface, effectively distributing weight more evenly across a larger area. Simultaneously, the mattress envelops the contours of the body, further reducing peak pressures on bony prominences. For instance, a patient lying in a supine position experiences a more uniform distribution of pressure across their back and buttocks, as the mattress conforms to their individual anatomy. This conformity helps to minimize areas of concentrated pressure that can lead to tissue breakdown. These features of immersion and envelopment can greatly reduce the pressure.
- Microclimate Control and Moisture Management
Excessive moisture contributes to skin maceration, increasing the risk of pressure injuries. A low air loss mattress typically incorporates a feature that gently circulates air, creating a microclimate that reduces moisture buildup on the skin’s surface. This is particularly beneficial for patients who are incontinent or perspire excessively. For example, the continuous airflow helps to wick away moisture from the skin, preventing it from becoming overly saturated and compromised. By maintaining a drier skin surface, the mattress enhances the skin’s resistance to friction and shear forces, further mitigating the risk of ulcer formation. A drier environment is a major component to pressure redistribution by increasing blood flow and decreasing risk of damage.
- Weight Capacity and Individualization
Effective pressure redistribution is contingent upon selecting a mattress with an appropriate weight capacity for the individual patient. Overloading the mattress can compromise its ability to provide adequate support and pressure relief. Additionally, some models allow for individualized pressure settings based on the patient’s weight and body composition. For example, a heavier patient may require higher inflation pressures to achieve optimal pressure redistribution. By tailoring the settings to the specific needs of the patient, th
e mattress ensures that pressure is effectively distributed across the support surface, regardless of their weight or size. Individualization of each patient helps maintain optimal health outcomes.
In summary, the pressure redistribution capabilities inherent in its design, encompassing alternating inflation/deflation, immersion/envelopment, microclimate control, and weight-specific adjustments, are crucial in preventing tissue damage in patients at risk for pressure injuries. The effectiveness of this intervention relies on proper patient selection, appropriate mattress settings, and adherence to a comprehensive skin care protocol.
2. Skin Microclimate
The skin microclimate, referring to the temperature and humidity immediately adjacent to the skin’s surface, plays a crucial role in maintaining skin integrity. In the context of patients utilizing hospital beds, particularly those with limited mobility, the microclimate is heavily influenced by the support surface employed. The relationship between the mattress system and this microenvironment is critical for pressure injury prevention.
- Temperature Regulation
An elevated skin temperature can increase metabolic demands and susceptibility to tissue damage. A low air loss mattress facilitates temperature regulation through the continuous circulation of air, dissipating heat and preventing localized hyperthermia. For instance, patients with fever or those confined to bed for extended periods are prone to increased skin temperatures. The airflow of the mattress system helps to mitigate this risk, maintaining a more stable and comfortable skin temperature. This is achieved by a constant, gentle breeze generated by the mattress’s internal air pump, preventing the skin from becoming excessively warm.
- Moisture Control
Excessive moisture, resulting from perspiration, incontinence, or wound exudate, can lead to skin maceration, weakening the skin’s barrier function and increasing its vulnerability to friction and shear forces. These mattresses employ airflow to wick away moisture from the skin surface, maintaining a drier environment. Consider a patient who is incontinent; the mattress’s airflow assists in drying the skin, preventing prolonged exposure to urine and reducing the likelihood of skin breakdown. This aspect of moisture control is vital in preventing moisture-associated skin damage (MASD).
- Oxygenation
While the primary function is pressure redistribution, some advanced models incorporate features that enhance oxygenation at the skin surface. Adequate oxygen supply is essential for cellular metabolism and tissue repair. By promoting airflow and reducing pressure on capillaries, these systems can indirectly contribute to improved oxygenation. For example, in areas where prolonged pressure might otherwise restrict blood flow, the alternating pressure and air circulation can help maintain tissue perfusion, facilitating oxygen delivery. This is achieved by ensuring that tissues under pressure are not deprived of vital oxygen.
- Influence on Skin pH
The skin’s pH, typically slightly acidic, plays a role in maintaining the skin’s barrier function and preventing bacterial colonization. Excessive moisture and certain topical agents can disrupt this pH balance. By maintaining a drier and more stable environment, the system helps to preserve the skin’s natural pH. An example would be a patient utilizing alkaline soaps; the mattress’s moisture control helps to prevent prolonged exposure to these soaps, thereby maintaining the skin’s optimal pH level. This is achieved by preventing excessive saturation of the skin, and this enhances the skin’s inherent ability to resist infection.
Therefore, the role of air circulation in these mattresses extends beyond mere pressure relief. By actively managing temperature, moisture, oxygenation, and influencing skin pH, it contributes significantly to maintaining a healthy skin microclimate. These systems are critical components in a holistic approach to pressure injury prevention, particularly for individuals at high risk due to immobility or other compromising factors. This is a critical aspect of quality patient care.
3. Patient Immobility
Prolonged immobility significantly elevates the risk of pressure injury development, necessitating specialized interventions to mitigate this risk. A low air loss mattress for a hospital bed directly addresses the challenges posed by immobility through pressure redistribution and microclimate control.
- Sustained Pressure and Ischemia
Immobile patients experience prolonged pressure on bony prominences, leading to tissue ischemia (reduced blood flow) and subsequent necrosis. A low air loss system actively cycles air, redistributing pressure away from vulnerable areas. For example, a patient unable to independently reposition experiences consistent pressure on the sacrum. The mattress’s alternating inflation and deflation cycles relieve this pressure, allowing for reperfusion and preventing tissue breakdown. This cyclical action is fundamental to its function.
- Compromised Skin Perfusion
Reduced mobility hinders natural blood flow regulation, exacerbating the impact of pressure. The therapeutic surface enhances perfusion through pressure redistribution and microclimate management. Consider a patient with spinal cord injury; impaired vasomotor control diminishes their ability to regulate blood flow. The support surface compensates by actively promoting circulation and preventing prolonged vasoconstriction in pressure-prone areas. This helps to alleviate the impairment.
- Increased Moisture and Maceration
Immobility can contribute to increased perspiration and incontinence, leading to moisture accumulation and skin maceration. A low air loss mattress facilitates moisture evaporation and ventilation, maintaining a drier skin surface. For instance, an immobile patient with excessive sweating is at increased risk of maceration. The system’s airflow wicks away moisture, preventing skin softening and breakdown. The airflow provides relief.
- Shear and Friction Forces
Immobile patients are vulnerable to shear and friction forces during repositioning or transfers. While the mattress does not directly eliminate these forces, its pressure redistribution properties reduce the overall vulnerability of the skin. For example, a patient sliding down in bed generates shear forces. By minimizing pressure concentration, the system reduces the likelihood of shear-induced tissue damage. This support aides during movement.
The benefits of the mattress are most pronounced when integrated with a comprehensive pressure injury prevention protocol. This includes regular skin assessments, nutritional support, and meticulous attention to moisture management. The appropriate surface contributes to a holistic approach for the immobile patient.
4. Ulcer Prevention
Pressure ulcers, also known as bedsores or pressure injuries, represent localized damage to the skin and underlying tissue, typically occurring over bony prominences. T
he etiology of these ulcers involves sustained pressure, shear forces, friction, and moisture, all of which compromise tissue perfusion and lead to cellular necrosis. A low air loss mattress for a hospital bed serves as a primary intervention strategy in ulcer prevention by mitigating these causative factors. The system’s alternating pressure cycles and air circulation reduce sustained pressure on vulnerable areas, improving blood flow and minimizing the risk of tissue breakdown. The implementation of such a mattress is therefore crucial in settings where patients are at high risk for developing pressure ulcers due to immobility, advanced age, or underlying medical conditions. For instance, in a long-term care facility, residents with limited mobility benefit significantly from this proactive approach, reducing the incidence of pressure ulcer formation and improving overall quality of life. The success relies on timely employment.
The connection between ulcer prevention and utilization is further reinforced by clinical evidence demonstrating the efficacy of these mattresses in reducing the incidence and severity of pressure ulcers. Studies have shown that incorporating these surfaces into a comprehensive prevention program, which includes regular skin assessments, nutritional support, and meticulous skin care, leads to substantial improvements in patient outcomes. In acute care settings, for example, patients recovering from surgery or suffering from critical illnesses are at elevated risk for pressure ulcer development. Employing the mattress as part of a multi-faceted prevention strategy can significantly decrease the likelihood of these complications, reducing hospital stays and associated healthcare costs. Early intervention is critical.
In summary, a low air loss mattress is a critical component of a comprehensive ulcer prevention strategy. Its ability to redistribute pressure, manage skin microclimate, and enhance tissue perfusion directly addresses the key etiological factors of pressure ulcer formation. While this system is not a standalone solution, its integration into a broader prevention program significantly reduces the incidence and severity of these debilitating conditions, ultimately improving patient outcomes and reducing the burden on healthcare resources. Proper selection, consistent monitoring, and adherence to manufacturer guidelines are essential for maximizing the benefits.
5. Inflation Settings
Appropriate adjustment of inflation parameters constitutes a critical determinant of efficacy for low air loss mattresses used on hospital beds. Incorrect settings can compromise pressure redistribution, negating the therapeutic benefits of the support surface and potentially increasing the risk of pressure injury development.
- Patient Weight and Body Mass Index (BMI)
The patient’s weight and BMI serve as primary indicators for establishing initial inflation levels. Manufacturers provide guidelines correlating weight ranges to specific pressure settings, ensuring that the mattress can adequately support the patient’s weight while effectively redistributing pressure. Overinflation can create a rigid surface, negating the pressure redistribution benefits, while underinflation may lead to bottoming out, concentrating pressure on bony prominences. For instance, a heavier patient with a higher BMI requires a higher inflation setting compared to a lighter patient with a lower BMI. Precise adjustment is imperative to ensure that the support surface delivers the intended therapeutic benefits, especially for patients with varying body compositions. Failure to follow these guidelines undermines pressure redistribution.
- Support Surface Monitoring and Adjustment
Ongoing monitoring of the surface and appropriate adjustments are essential for optimal performance. Factors such as changes in patient weight, the use of additional support devices, or variations in bed position may necessitate adjustments to the inflation settings. Regular visual inspection of the surface to confirm that the patient is not bottoming out is important. If the patient’s bony prominences are making contact with the underlying bed frame, the inflation setting needs to be increased. It may also be necessary to consult a qualified healthcare professional for guidance on making adjustments to achieve optimal pressure redistribution. Regular assessment and adaptation help ensure effective long-term use.
- Mattress Model Specifications and Manufacturer Guidelines
Different models of low air loss mattresses may have distinct inflation mechanisms and setting ranges. Adhering to the manufacturer’s guidelines is crucial for safe and effective operation. Some mattresses may offer manual inflation adjustments, while others feature automated pressure regulation based on patient weight. Understanding the specific capabilities and limitations of the selected mattress model is essential for accurate inflation setting. For example, utilizing a setting outside the recommended range may compromise the mattress’s functionality. Compliance with manufacturer specifications ensures proper operation.
In summary, the meticulous adjustment of inflation parameters, informed by patient-specific characteristics, ongoing monitoring, and adherence to manufacturer guidelines, are all essential elements for maximizing the clinical benefits of such systems. Appropriate application promotes optimal pressure redistribution, mitigating the risk of pressure injury development in vulnerable patients.
6. Maintenance Protocol
The effectiveness and longevity of a low air loss mattress for a hospital bed are directly contingent upon adherence to a rigorous maintenance protocol. Neglecting proper maintenance can compromise the mattress’s therapeutic capabilities, increase the risk of infection, and shorten its lifespan, ultimately affecting patient outcomes and increasing healthcare costs.
- Regular Cleaning and Disinfection
Routine cleaning and disinfection are paramount for infection control. Body fluids, wound exudate, and other contaminants can compromise the integrity of the mattress cover and create a breeding ground for pathogens. Cleaning should be performed regularly using approved disinfectants, following manufacturer guidelines. Failure to properly disinfect after each patient use increases the risk of cross-contamination. For example, neglecting to remove visible soiling or using inappropriate cleaning agents can damage the mattress material, compromising its protective barrier and necessitating premature replacement.
- Inspection for Damage and Wear
Regular inspection for tears, punctures, or other damage to the mattress cover is essential. Compromised covers can allow fluids to penetrate the interior, leading to bacterial growth and reduced effectiveness. Routine inspection should include checking seams, zippers, and air cell connections for signs of wear or leakage. For instance, a small tear in the cover, if left unaddressed, can quickly expand, rendering the mattress unusable. Prompt repair or replacement of damaged components is crucial to maintaining its integrity and functionality. A small needle poke can result in significant harm if not identified.
- Air Pump and Filter Maintenance
The air pump is the heart of the low air loss system, responsible for maintaining pressure and airflow. Routine mainten
ance includes checking the pump for proper operation, cleaning or replacing air filters, and inspecting electrical cords for damage. Clogged filters can reduce airflow, diminishing the mattress’s pressure redistribution capabilities. For example, a pump operating with a dirty filter may overheat or fail prematurely, disrupting the mattress’s pressure regulation. Adhering to the manufacturer’s recommended maintenance schedule for the pump is critical for ensuring consistent and reliable operation. - Storage and Handling Procedures
Proper storage and handling practices are essential for preventing damage to the mattress when not in use. Mattresses should be stored in a clean, dry environment, protected from direct sunlight and extreme temperatures. Avoid stacking heavy objects on top of the mattress, as this can damage the internal air cells. When transporting the mattress, ensure that it is properly supported to prevent tearing or punctures. Improper storage can lead to deterioration of the mattress material, reducing its effectiveness and lifespan. Fold carefully to avoid damage.
In conclusion, adherence to a comprehensive maintenance protocol is indispensable for preserving the functionality, safety, and therapeutic benefits of a low air loss mattress for a hospital bed. Regular cleaning, thorough inspections, proper pump maintenance, and appropriate storage procedures are essential for maximizing the investment in this critical piece of medical equipment and ensuring optimal patient outcomes.
Frequently Asked Questions Regarding Low Air Loss Mattresses for Hospital Beds
This section addresses common inquiries concerning the proper application, maintenance, and expected performance of these specialized support surfaces.
Question 1: What constitutes an appropriate candidate for a low air loss mattress?
Individuals at high risk for pressure injury development due to immobility, compromised skin integrity, poor nutritional status, or existing pressure ulcers are generally considered appropriate candidates. A thorough risk assessment is essential to determine suitability.
Question 2: How often should a low air loss mattress be cleaned and disinfected?
The mattress should be cleaned and disinfected between each patient use, as well as periodically during extended use by the same patient. Adherence to established infection control protocols is crucial.
Question 3: What is the expected lifespan of a low air loss mattress?
The lifespan varies depending on the quality of the mattress, the frequency of use, and the diligence of maintenance procedures. A well-maintained mattress can typically last for several years under normal conditions.
Question 4: Can a standard hospital bed be used with a low air loss mattress?
Yes, these mattresses are generally designed to fit standard hospital beds. However, it is essential to verify compatibility with the specific bed frame to ensure proper support and functionality.
Question 5: What are the potential risks associated with using a low air loss mattress?
Potential risks include electrical hazards (if the pump is damaged or improperly grounded), skin irritation due to cover materials, and the possibility of bottoming out if the mattress is not properly inflated or maintained.
Question 6: Are low air loss mattresses effective for treating existing pressure ulcers?
While these mattresses can aid in the healing of existing pressure ulcers by reducing pressure and improving blood flow, they should be used in conjunction with a comprehensive wound care protocol, including proper wound cleansing, debridement, and dressing application.
The information provided herein serves as a general guide and should not replace the advice of qualified healthcare professionals. Consultation with a physician or wound care specialist is recommended for specific patient needs.
The subsequent section will provide a summary of key considerations.
Conclusion
The preceding exploration has illuminated the critical role of the low air loss mattress for hospital bed applications. Key aspects, including pressure redistribution, microclimate control, and the mitigation of risks associated with patient immobility, underscore its significance in pressure injury prevention and management. Proper patient selection, adherence to recommended inflation settings, and diligent maintenance protocols are crucial for maximizing the therapeutic benefits and ensuring the longevity of these specialized support surfaces.
The information presented serves as a foundation for informed decision-making regarding the integration of this important technology into comprehensive patient care plans. Continued research and vigilance are essential to optimizing its application and improving patient outcomes in the ongoing effort to combat pressure injuries across diverse healthcare settings. The responsible implementation of these systems is a critical component of quality patient care.


![Best Camper Bunk Bed Mattress [RV Comfort!] Organic & Natural Mattress Buyer’s Guide: Non-Toxic Sleep Solutions Best Camper Bunk Bed Mattress [RV Comfort!] | Organic & Natural Mattress Buyer’s Guide: Non-Toxic Sleep Solutions](https://mattressworldpa.com/wp-content/uploads/2025/07/th-7217-300x200.jpg)

![Space-Saving Mattress Firm Murphy Bed [Deals!] Organic & Natural Mattress Buyer’s Guide: Non-Toxic Sleep Solutions Space-Saving Mattress Firm Murphy Bed [Deals!] | Organic & Natural Mattress Buyer’s Guide: Non-Toxic Sleep Solutions](https://mattressworldpa.com/wp-content/uploads/2025/07/th-7215-300x200.jpg)